Single State MtF Gender Reassignment Surgery
Conference Name: Gender Reassignment- MtF
Conducted by: Dr. Sanjay Pandey
Surgeon(s)/Speaker(s): Dr. Sanjay Pandey
Surgical Procedure: Urology-Gender Reassignment MtF
Location: Kokilaben Dhirubhai Ambani Hospital and research Institute Mumbai
Indexsteps
1. Social Lithotomy Position : Patient in social lithotomy position with pressure points safeguarded and pneumatic compression on calves.
2. Painting and Draping : Under all aseptic precautions, painting and draping done with anal verge kept in the operating field for monitoring posterior dissection.
3. Marking Perineal Flap : Perineal flap marked upto the root of the shaft as a large tongue shaped flap to encompass posterior vaginal wall; the incision is deepened to the Colles’ fascia to maintain vascularity and raised till approx 1 inch from the anal verge. ( landmarks – Bilateral Ischial Tuberosities)
4. Bilateral Orchidectomy : Bilateral orchidectomy done preserving the overlying scrotal fat towards cushion creation for future labia.
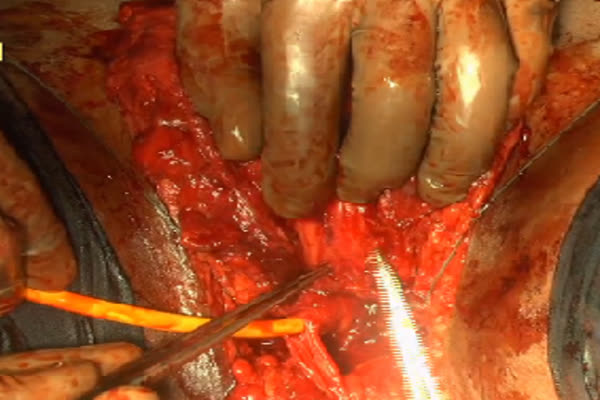
5. Blunt and Sharp Dissection : Blunt and sharp dissection done between posterior urethra and rectum to create space for neovagina along the anterior rectal wall upto the base of the prostate, guided by rectal finger.
6. Circumcoronal Penile Incision : Circumcoronal penile incision deepened till the level of Buck‘s fascia; Penile degloving done in the right plane.
7. Creation of Anterior wall of Neovagina : Penile skin flap split ventrally in midline and mobilized upto pubic symphysis for creation of anterior wall of neovagina.
8. Penile Disassembly : Penile disassembly commenced circumferentially from the periurethral zone on the ventral aspect along entire length.
9. Neurovascular Bundles : Neurovascular bundles preserved from root of penis to glans.
10. Formation of Clitoris : Dorsal portion of glans is used for formation of clitoris with adequate vascularity.
11. Corporal Bodies Mobilization : Corporal bodies mobilized ‘completely’ shaved from the bones with adequate haemostasis.
12. Endostitch : Neovaginal space pack removed towards assessing hemostasis and the future vaginal apex fixation stitches to the sacro spinal ligaments bilaterally with Endostitch is completed.
13. Vagina Creation : Upper and lower skin flap used to create vagina by continuous PDS 3 - 0 sutures, marking the apex of the vaginal vault.
14. Mons Pubis : Neoclitoris and the urethra are transposed dorsally through the midline incision on the penile flap to create a mound of Mons pubis and place the clitoris and urethra sequentially
15. Urethra Spatulation : Urethra spatulated dorsally and hemostasis achieved of the spongy bulb, neomeatus created as a perineal urethrostomy of satisfactory positioning
16. Neoclitoris : Neoclitoris is “strategically” positioned and fixed to the periosteum.
17. Vaginal Depth : Satisfactory vaginal depth of approximately 4-6 inches as needed with vertical axis accepting the largest vaginal mould with ease: Penultimate mould is left in place as a additional hemostatic mechanism towards final position and shape of the vaginal canal.
18. Labia majora and labia minora : Labia majora is created from residual penoscrotal skin with symmetry; labia minora was created from the base of the penile shaft skin.
19. External hemostasis : External hemostasis checked, symmetry assured, mould placed.
20. Placing compression dressing : Compression dressing placed with 16Fr catheter in situ and a drain in the perivaginal space.
21. Dressing : Dressing done.
pre_post_measures
1. Preoperative investigations : Complete blood count :new:Blood Sugar :new:Renal Function Tests :new:Liver Function Tests :new:Coagulation Profile :new:HIV/ HbsAg / Anti HCV (Hospital Mandatory) :new:Blood Group :new:Chest X-Ray :new:ECG :new:Echocardiogram ( for all in view of hormonal replacement therapy ) :new:Abdominal and Pelvic USG
2. Preoperative measures : Overnight polyethylene glycol ( PEG ) for bowel preparation :new:Patient catheterised to empty bladder :new:Attachement of diathermy
Surgical Instruments
1. Open General operative set
2. Endostitch
3. Fixation device